by Lara Pizzorno, MDiv, MA, LMT with Barry Wheeler, ND
Treating the sequelae of andropause, the age- and stress-related decline in hormones in the adult male, with bio-identical hormone replacement (BHRT) can restore more youthful hormone levels and significantly alleviate symptoms associated with “normal” aging, optimizing health, happiness and quality of life. Successful and safe BHRT, however, necessitates laboratory testing to assess the patient’s current hormonal status, monitor treatment, and ensure that he is metabolizing hormones in ways that reduce his risks for prostate cancer, cardiovascular disease, metabolic syndrome, osteoporosis, and the “low grade” depression often seen in older men, as well as declines in cognitive and sexual function.
As discussed in detail in Part I of this review and recapped briefly here in relation to the male patient, hormones can be assayed using saliva, blood (serum), and urine. Which of the three hormone test methods, or which combination of tests, you will wish to utilize will depend upon what information you require in a given clinical situation.
Salivary Hormone Testing
Advantages
In males, saliva testing may be helpful for monitoring cortisol circadian rhythm. For the four-point (6am, 12pm, 6pm, and 12am) cortisol assay required to evaluate cortisol circadian rhythm, salivary testing is the only practical option.
Disadvantages
While saliva testing can help determine the circadian rhythm of cortisol, it cannot provide information on tetrahydrocortisol (THE), tetrahydrocortisone (THF), and allo-tetrahydrocortsiol (5a-THF) levels, which is needed to determine adrenal reserve, 1 ,2 and thus, whether prescribing herbs, such as licorice, withania somiferum (ashwaganda), Panax ginseng or others, will be potentially beneficial or if replacement with hydrocortisone is indicated. Furthermore, it is difficult to estimate total production of cortisol since a night time spike, which is common in those with sleep disturbances, may be missed.
As discussed in detail in Part I of this review, salivary testing has repeatedly been shown to be highly unreliable for testosterone.
Like serum testing, saliva tests offer only a ‘snapshot’ look at hormones that ebb and flow throughout a 24-hour period, for which reason its diagnostic value for testosterone, estradiol, progesterone, dehydroepiandrosterone (DHEA) and aldosterone is compromised by rapid fluctuations in salivary concentrations of these steroids. Samples would need to be taken multiple times throughout the day and night to obtain reliable information.
More importantly, saliva tests cannot capture hormone metabolites, so cannot provide the clinician with information essential to safe hormone replacement therapy, e.g.:
- What percentage of testosterone is being converted into 5α-DHT, and from there through 5α-androstanediol into 5α-androstane-3α,17β-diol (aka 3α-adiol, a storage form of 5α-DHT) and 5β-androstane-3α,17β-diol (aka 3β-adiol, a cancer-preventive metabolite.) A newly available serum Testosterone Metabolites test, discussed below, assesses these metabolites.
- The activity level of 5α-reductase (5AR), the enzyme that converts testosterone to 5α-DHT. Excessive 5AR activity promotes benign prostatic hypertrophy and male pattern baldness; however, under activity of this enzyme can promote prostate cancer since inhibition of 5α-DHT production will also inhibit production of its protective metabolite, 3β-adiol.
- Levels of metabolites that indicate the extent of adrenal reserve or fatigue, e.g., tetrahydrocortisone (THE), allotetrahydrocortisol (5α-THF), tetrahydrocortisol (THF), allotetrahydrocorticosterone (5α-THB), tetrehydrocorticosterone (THB), 11-dehydrotetrahydrocorticosterone (THA). These metabolites are reported by the 24-Hour Urine test (discussed with a focus on women in Part I of this review and summarized in relation to men below).
In sum, in the male patient, salivary steroid testing may be useful for assessing circadian patterns for cortisol. For this indication, collection of unstimulated saliva into small plain tubes and storage at −20° C is recommended to avoid known pitfalls (See Part I). Saliva testing is not a reliable option for even a snapshot evaluation of androgen levels.
Blood (Serum) Hormone Tests
Advantages
Serum testing offers a reliable and is the preferred option for testing a number of hormones including:
- Luteinizing Hormone (LH) – low levels may indicate excessive aromatization if low LH accompanies a decrease in the testosterone : estradiol ratio, as this would suggest suppression of testosterone production by estradiol (via the negative feedback loop in which estradiol inhibits GnRH and therefore LH release from the pituitary). Low LH (especially the few seen at unfindable levels or close) may also indicate a “central” (pitutitary) reason for low or low normal serum testosterone levels, which is often improved by injection of HCG.3 , 4
- Thyroid Stimulating Hormone (TSH)
- Reverse T3
- Insulin
- Dihydrotestosterone (DHT)
Measurement of these compounds in serum is the best choice because most are proteins and thus do not show up in urine in significant quantities if the kidneys are functioning normally. Others, e.g., reverse T3, are extremely small, and thus more easily measured in serum than urine. Additionally, DHT, which is very difficult to measure in any medium, is most accurately measured in serum using high-performance liquid chromatography-tandem mass spectrometry (LC-MS/MS).5 , 6
Disadvantages
Serum hormone tests directly assess the amount of hormones in the circulation; however, significant limitations must be noted.
Most important is that measurement of sex hormones in serum is necessarily a ‘snapshot’ peek at hormones that fluctuate significantly during the day both pre-andropause and in men using any form of hormone replacement therapy (as indicated by Figure 1 below). The testes, in which Leydig cells produce 95% of the body’s testosterone, secrete hormones in pulses throughout the day. In men given testosterone injections, levels increase dramatically, peak within two to four days, then drop rapidly. Men supplemented with natural testosterone may be applying transdermal creams or gels once or twice daily or may be using a patch or sublingual tablet; regardless of the delivery form chosen, testosterone levels will fluctuate throughout the day.
Figure 1: Serum Testosterone Concentration: Differences Among 3 Delivery Forms
- A) During 14 days following the injection of 200 mg of testosterone enanthate.
B) During the 24 hours after application of one or two testosterone patches that
deliver approximately 5 mg of testosterone each. C) During the 24 hours after
application of a testosterone gel containing 50 or 100 mg of testosterone. Figure from Testosterone treatment of male hypogonadism, UptoDate in Endocrinology, www.uptodate.com,
accessed 1-15-11.References used to develop Figure 1 7, 8 ,9 , 10 , 11
Adding to the “snapshot” limitation is the fact that — with the exception of testosterone for which both free and total values are typically reported — most serum tests report only “total” hormone values, i.e., the sum of free, conjugated and bound forms of the hormones. Free estrone, free estradiol, and free progesterone are rarely measured in serum. In men, the ratio of free testosterone : free estrogens should be ≥4. If <4, this indicates excessive aromatization and possible insulin resistance.
Another distinction not taken into consideration in serum tests is that among free, conjugated and bound forms. Bound forms have been completely inactivated, but conjugated steroids (which have combined with simple molecules, i.e., glucuronic acid or sulfates in Phase II liver conjugation) can be activated by glucuronidases and sulfatases. Sulfatases are not only highly prevalent in breast tissue in men as well as women, but are also found in numerous other tissues including prostate bone, and brain. Quantitative data show that the sulfatase pathway, which transforms estrogen sulfates into bioactive unconjugated estradiol, is actually 100–500 times more active than the aromatase pathway, which converts androgens into estrogens. Thus, the distinction between conjugated and bound forms of estradiol is clinically important in men since the sulfatase pathway is a significant contributor to body load of bioactive estradiol. Conjugated estradiol is a factor in estrogen-related prostate cancer (via its potential for metabolism to 16α-OH estrone).12
In addition, conjugated estrogens can be re-activated in the intestines and returned to circulation via the action of beta-glucuronidase enzymes, which are produced by E. coli, Clostridum and Bacteroides 13 ; thus intestinal dysbiosis may increase a man’s circulating levels of active estrogens). For these reasons, evaluation of hormone replacement therapy in men should assess not only testosterone, but both free and conjugated estrogens. The 24-hour Urine Test does so; serum tests do not.
As a consequence of all of the above, serum testing does not provide the clinician with adequate information to safely prescribe or evaluate the effects of androgen replacement therapy. For example, an andropausal man whose serum test results indicate total testosterone at normal levels may still be experiencing loss of muscle and libido, prostate enlargement, and erectile dysfunction, along with increased risk of cardiovascular disease, osteoporosis and depression, if most of his testosterone is bound, which becomes increasingly likely in men >50, the age at which testosterone levels typically begin to decline, while levels of sex hormone binding globulin (SHBG) increase with age.14
Prescribing testosterone to this patient to alleviate his symptoms may result in increasing his levels of estradiol if his aromatase enzyme, which readily converts testosterone to estradiol, is overactive. Excessive aromatization, in addition to its “feminizing” effects, may increase prostate cancer risk since estradiol can be metabolized to estrone, which can then be converted to either protective 2-hydroxyestrone (2-OH) or Estriol (E3) OR into potentially pro-carcinogenic 16α-OH estrone. On the other hand, insufficient aromatization not only promotes bone loss in men since some 16α-OH is required for bone remodeling, but has recently been shown to promote prostate cancer by inhibiting the production of 3β-adiol (discussed next). Serum testing will not indicate which estrogen metabolites a man is producing.
When testing male hormones in serum, a morning blood draw is recommended since that is when they are typically at their highest levels. More typically, serum free testosterone will be low in an adropausal man experiencing the symptoms noted above. Nevertheless, to reduce risks, more information is needed than typical serum testing can provide.
Testosterone Metabolites Serum Testing
A recently developed serum test, the Testosterone Metabolites Profile, does provide significant insight into prostate cancer risk, however. This test captures levels of not only 5α-DHT, but its metabolites: 5α-Androstane-3α-17β-diol (aka 3α-adiol) and 5α-Androstane-3β-17β-diol (aka 3β-adiol).
Low levels of 5α-DHT are indicative of over-inhibition of 5α-reductase (5AR), the enzyme that converts testosterone to 5α-DHT, which is ~2-3 times as potent as testosterone due to 5α-DHT’s greater affinity for androgen receptors.15
Drugs designed to inhibit 5AR (e.g., finasteride [Propecia, Proscar], dutasteride [Avodart]) and botanical supplements (e.g., Serenoa repens [Saw palmetto]) are taken by hundreds of thousands of men around the world to combat benign prostatic hypertrophy and androgenic alopecia (male pattern baldness). It has also been assumed that 5α-DHT is a key contributor to prostate cancer initiation and progression, so 5AR inhibitors are commonly used to treat prostate cancer. However, recent studies show a correlation between low levels of DHT and decreased survival in prostate cancer patients, rendering this assumption highly questionable.16 ,17 , 18 , 19 According to one recent paper, “Low dihydrotestosterone in the prostate is probably sufficient to propagate the growth of aggressive prostate cancer.” 20
The American Society of Clinical Oncology/American Urological Association 2008 Clinical Practice Guideline states: “Men who are taking 5-ARIs for benign conditions such as lower urinary tract symptoms (LUTS) may benefit from…understanding that the improvement of LUTS relief should be weighed with the potential risks of high-grade prostate cancer from 5-ARIs.” 21
Mechanisms through which 5α-reductase inhibitors promote prostate cancer
Over-inhibition of 5AR results in increased availability of testosterone, which may be shunted, via aromatase, to estradiol, causing “feminization,” e.g., gynecomastia, one of the side effects of 5AR inhibitor drugs; and decreased production of not only 5α-DHT, but its metabolites, 5α-Androstane-3α-17β-diol (aka 3α-adiol, a storage form of 5α-DHT), and 5α-Androstane-3β-17β-diol (aka 3β-adiol), an estrogen receptor beta (ERβ) ligand that promotes normal cellular differentiation, thus lessening risk of benign prostatic hypertrophy and prostate cancer.22 ,23, 24
ERβ is involved in several biological functions in the prostate, including regulation of cell proliferation, apoptosis and differentiation. 3β-adiol, as an alternative ligand to estradiol of ERβ (the concentration of 3β-adiol in prostate is 100-fold higher than that of estradiol), mediates the majority of these effects. ERβ expression has been revealed to be greatly decreased in malignant prostate tissue, reaching nearly undetectable levels with tumor progression in more than 75% of cases. Reintroduction of ERβ triggers apoptosis, and decreases proliferation and invasiveness of malignant cells. In addition, prostate hyperplasia has also been described in mice lacking ERβ, and 3β-adiol has been shown to more potently induce expression of ERβ in the rat prostate than estradiol or 5α-DHT.23
3β-adiol has lately also been revealed to be a key means through which the neuroendocrine response to stress is modulated in males. 3β-adiol suppresses excessive hypothalamic-pituitary-adrenal (HPA) axis activation, which would otherwise promote depression and neurodegeneration.25 , 26
Balancing Men’s Hormones Summary:
Issues to Consider
Under activity of 5α-Reductase (5AR):
- Since 5AR is the enzyme that converts testosterone to 5α-DHT, excessive 5AR activity promotes benign prostatic hypertrophy and male pattern baldness; however, 5AR underactivity will inhibit 5α-DHT production, and therefore production of its protective metabolite, 3β-adiol, and thus can promote prostate cancer.
- Solution—check for 5AR inhibitors and reduce or eliminate. Increase 5AR expression with exercise. Increase 5AR activity with DHEA and free testosterone; both upregulate 5AR activity in the prostate. Check free testosterone levels via 24 Hour Urine test; SHBG increases after age 50, resulting in decreased levels of free testosterone, so serum levels (total testosterone) in “normal” range do not confirm adequacy.
Over activity of 5α-Reductase:
- If levels of androsterone are high on the 24 Hour Urine test, this may indicate that 5AR activity is elevated, especially if androsterone is high in relation to etiocholanolone. Excessive DHEA supplementation (>50mg/day in males) is a possible cause.
- Solution—if 5AR activity is excessive, it may be lessened by zinc, Gamma-linolenic (GLA), docosahexaenoic acid (DHA), green tea extract, saw palmetto, and progesterone; and will be strongly inhibited by finasteride and dutasteride.
- The nutrients (GLA, DHA, vitamin D3, and zinc) are unlikely to cause over-inhibition of 5AR and are suggested to use to replace the more potent “patent drugs” like finasteride. Also since these nutrients are required by the body, it is preferable not to decrease their intake (unless excessive), but to add Myomin and/or address the insulin resistance with diet and exercise.
- Always recheck within 3 months to ensure over-inhibition has not occurred since 5AR over-inhibition can promote aggressive prostate cancer.
Excessive aromatization:
- Excessive testosterone supplementation (≥75 mg/day) can result in excessive aromatase activity and elevated total estrogens in men.
- Excessive aromatase activity is almost always associated with insulin resistance. Check for insulin resistance.
- Solution: In addition to diet and exercise, supplementation with vitamin D, chromium, (if patient is insulin-resistant & when combined with biotin), and berberine .
- Solution: Myomin (2 to 3 capsules BID) and Chrysin (liposomal drops, 6 drops sublingually BID) will also lessen aromatase activity.
- Use of 5AR inhibitors may also result in excessive aromatization. 5AR inhibitors include not only the drugs Finasteride (Proscar, Propecia) and Dutasteride (Avodart), but the botanical medicine, Serenoa repens (Saw palmetto); the nutrients, Gamma-linolenic acid (GLA) ,Eicosapentaenoic acid (EPA), Alpha-linoleic acid, and Oleic acid (olive oil); Progesterone , and heavy metals, e.g., cadmium and arsenic.
- Solution: Check for use of Finasteride (Proscar, Propecia), Dutasteride (Avodart), Saw palmetto and reduce dosage or discontinue. Check for excessive intake of GLA, EPA, ALA, olive oil and lessen intake. Check for heavy metals and promote detoxification with NAC, DMSA, and infared sauna if indicated.
- Also check cortisol levels; in excess, cortisol promotes insulin resistance and many features of the metabolic syndrome (e.g., glucose intolerance, hypertension, dyslipidemia).
- Retest with 24-Hour Urine after 3 months to ensure sufficient 16α-OH estrone is present for bone health; run Serum Testosterone Metabolites to check 3β-adiol
- One indication of excessive aromatization would be low Lutenizing Hormone (should be checked with serum test) – if accompanied by a decrease in the testosterone : estradiol ratio (as shown on a 24 Hour Urine) – as this would suggest suppression of testosterone by estradiol and thus excessive aromatization.
Dysbiosis:
- Conjugated estrogens can be re-activated in the intestines and returned to circulation via the action of beta-glucuronidase enzymes, which are produced by E. coli, Clostridum and Bacteroides ; thus intestinal dysbiosis may increase a man’s circulating levels of active estrogens. This would be seen as a decrease in the testosterone : estradiol ratio (as shown on a 24 Hour Urine).
- Solution – run Comprehensive Digestive Stool Analysis to identify pathogens. Use Institute for Functional Medicine “5 R” Program (available at http://www.functionalmedicine.org/ ):
- Remove toxins: i.e., allergic foods, parasites, pathogenic bacteria or yeast overgrowth). This might involve using an allergy “elimination diet” or prescribing drugs or herbs to eradicate a particular bug. It might also involve making healthier dietary choices: a whole foods, Mediterranean style, lower carb diet; less processed, high glycemic index foods.
- Replace: replace digestive enzymes, hydrochloric acid and bile acids whose secretion may have been compromised by diet, drugs, diseases, aging.
- Reinoculate: with probiotic foods (e.g., yogurt with active cultures), supplements that contain bifidobacteria and lactobacillus species, and consumption of the high soluble fiber foods that contain fructooligosaccharides (FOS) and other prebiotics.
- Repair: supplement with key nutrients utilized by GI tract cells for repair, e.g., zinc; vitamins A, C, and E; fish oil; glutamine.
- Rebalance: lifestyle choices – sleep, exercise and stress — can all affect the GI tract.
Imbalanced 2/16α ratio:
- While conversion of some estrone to 16α is required for bone health, high levels of 16α, which promote prostate cancer, are caused by obesity, hypothyroidism, pesticides, alcohol and cimetidine.
- Estrone’s conversion to (cancer preventive) 2-OH estrone is promoted by indole-3-carbinol (I3C), 3.3- diindoylmethane (DIM), flax, soy, omega-3 fatty acids and exercise.
- Levels of 16a-OH E1 can also be lowered by increasing its conversion to estriol. This conversion is stimulated by iodine and iodide.
- Supplementation with Calcium D-glucarate supports proper elimination of estrogen by inhibiting beta-glucuronidase, an enzyme produced by colonic microflora (e.g., E.coli) that hydrolyzes glucuronide conjugates, thus returning estrogen into circulation. (The major route of estrogen elimination in humans is through Phase II glucuronidation in the liver.)
Promoting 3β-adiol Production
Monitor Impact of All 5α-Reductase Inhibitors
Given the importance of 3β-adiol for prostate cancer prevention, stress reduction and prevention of age-related cognitive decline, men using any type of 5AR inhibitor — natural compounds as well as patent medicines — should be monitored for over-inhibition. If over-inhibition is found: (1) use a lower dose of, or a less potent, 5AR inhibitor (2) replace 3β-adiol by asking your compounding pharmacy to include it in your patient’s testosterone cream.27
5α-Reductase Inhibitors
- Finasteride (Proscar, Propecia)
- Dutasteride (Avodart)
- Serenoa repens (Saw palmetto)28
- Gamma-linolenic acid (GLA)29
- Eicosapentaenoic acid (EPA)29
- Alpha-linoleic acid30
- Oleic acid (olive oil)30
- Progesterone31
- Heavy metals, e.g., cadmium and arsenic32, 33
5α-Reductase Agonists
DHEA as well as free testosterone upregulates 5AR activity in the prostate34, 35; levels of both are assessed on a 24-Hour Urine Hormone Profile.
Exercise, even a single session on a treadmill, significantly increases 5AR expression—at least in male and female mice. 36
Indirect Assessment of 5α-Reductase Activity
A 24-Hour Urine test provides two ratios that assess 5AR activity: Andosterone:Etiocholanone and Allo-tetrahydro-cortisol:Tetrahydro-cortisol. These are discussed in Part II of this review.
Very low ratios of the above hormones in urine indicate low 5AR activity and are suggestive of very low 5α-DHT production. Follow-up testing with a serum Testosterone Metabolites Profile can confirm since serum testing, which allows assessment of two other important ratios: the ratio of Testosterone:5α-DHT and that of 5α-DHT:3β-adiol, is a better indicator of elevated, low or normal levels of DHT.
The serum Testosterone Metabolites Profile also allows assessment of two other important ratios: the ratio of Testosterone:5α-DHT and that of 5α-DHT:3β-adiol:
Testosterone:5α-DHT: In men, (average age 64 +/- 9 years), a higher testosterone to 5α-DHT ratio has been associated with a 42% decreased risk of BPH.37 A significant inverse association has also been shown between Testosterone:5α-DHT and lower urinary tract symptoms (LUTS). Additionally, men with higher concentrations of bioavailable testosterone had a 56% decreased risk of LUTS compared with those with hypogonadal concentrations.38
As early as 1966, a study found an inverse relationship between tumor volume and the testosterone : DHT ratio in men screened for prostate cancer. Lower DHT values were seen in more advanced tumors. Testosterone levels were also lower in patients with cancer than in the control group. An inverse relationship was also found between tumor volume and 5α-DHT level; 5α-DHT levels tended to be lower among cases and in those with more advanced tumors, and the testosterone : 5α-DHT ratio was higher in patients with more advanced tumors.39
More recently, a 2008 study found that plasma 5α-DHT levels were reduced when testosterone was given to elderly men with below normal levels of testosterone and elevated 5α-DHT levels at baseline. 40
Several possible mechanisms could explain why: (1) Since 5α-DHT is ~3x as potent as testosterone, 5α-reductase activity may be increased to compensate for the low testosterone levels pre-treatment. When testosterone is given, the need to compensate via increased production of 5α-DHT is removed; the androgen receptors are now also being activated by testosterone, resulting in signaling for reduced synthesis of 5α-reductase and/or reduced 5α-reductase activity.41 In sum, the research suggests that testosterone replacement promotes normalization of 5α-reductase activity, 5α-DHT levels and its metabolism to 3β-adiol.
5α-DHT : 3β-adiol : While 5α-DHT has been seen only as a potential promoter of proliferation and growth in the prostate, its metabolite 3β-adiol is a differentiating agent that activates ERβ and may help prevent cancer. A growing body of evidence suggests that the ratio of 5α-DHT to 3β-adiol may much more important than their absolute values.22,23,24,42 However, the ratio of 3β-adiol : (5a DHT + 3α-adiol) may be even more useful since 3α-adiol serves as a “reservoir” which re-cycles back to 5α-DHT.23
Urine Hormone Testing
Advantages
- The 24-Hour Urine sample may be relied upon to accurately evaluate and monitor:
- Total daily production of hormones
- Free androgens (DHEA & testosterone)
- Androgen balance
- Androgen metabolites (new serum tests provide information on additional analytes not reported in urine testing)
- Male female sex hormone balance and metabolites
- Activity of the 5α-reductase and aromatase enzymes
- Prostate cancer hormonal risk factors (e.g., in men, the 2:16α ratio, the Testosterone:Estrogen ratio [low T:E suggests insulin resistance which correlates with increased risk for prostate cancer])
- Liver function as indicated by assessment of Phase I and II metabolites
- Human growth hormone
- Adrenal health / adrenal reserves
As discussed in Part II of this review, urine hormone testing using both gas chromatography-mass spectrometry (GS-MS) or liquid chromatography-tandem mass spectrometry (LC-MS/MS) is well-established in the medical literature as a reliable method of assessing levels of active (free & conjugated) hormones and their metabolites, correlates well with patient symptoms, and reflects the beneficial impact (or lack of benefit and potentially oncogenic effect) of therapeutic interventions.43, 444 Radioimmunoassay (RIA) and enzyme-linked immunosorbent assay (ELISA, also known as enzyme immunoassay [EIA]) analysis may not be accurate. The clinical takeaway: ask the lab you use what procedures they are using.45, 46, 47
A 24-hour urine sample is non-invasive, easy for the patient, and provides a more accurate indication of hormonal output since it averages out the hour-to-hour fluctuations seen in both serum and salivary measurements.
In addition, a 24-Hour Urine test captures metabolites that are not measurable in saliva and cannot be reliably measured by a single, or even multiple, blood draws, e.g., 16α-OH estrone, an estrogen metabolite shown to impact bone loss in men, and a number of glucocorticoid and mineralocorticoid metabolites (discussed in Part II of this review) that provide greater insight into long-term adrenal health, short term stress response, the cortisol/cortisone balance, and other measures of adrenal health and function than assessment of cortisol alone.
Disadvantages
Circadian fluctuation of cortisol cannot be measured using 24-hour urine collection. To prevent sample contamination, patients applying transdermal cream to the scrotum or testicles should be instructed to apply to the perianal mucosal area on the day of collection.
The 24-Hour Urine Test: Analyte Interpretation and Evaluation for Men
Following is an explanatory listing of the steroids evaluated by the most comprehensive of the 24-hour urine tests, the Comprehensive PLUS Hormone Profile with hGH. Levels of all steroids reported indicate free plus conjugated forms.
For a schematic overview of the metabolism of these steroids, please see Part II of this review, Figure 1: “Metabolism of Select Steroids.”
24 Hour Urine Test analytes and adult reference ranges for men are summarized in Figure 2 below.
24 Hour Urine Test Analytes
Creatinine: a break-down product of creatine phosphate in muscle, which is produced by the body at a fairly constant rate and filtered out of the blood by the kidneys. Creatinine concentration provides a marker for a full – neither under nor over – urine collection.
The adult reference range is 0.5 – 2.0 gm/24hr. Since it is a muscle breakdown product, creatinine is typically higher in men than women (especially if the patient exercised on the day of collection).
Total urine volume: ranges from 1,200 – 3,000 mL; most likely to be ≥1,500 in men.
SEX HORMONES: ESTROGENS
Estrone (E1): The most potent estrogen, estrone is derived from testosterone via prior aromatization to estradiol and estradiol’s conversion by 17β-hydroxysteroid dehydrogenase (17β-HSD) to estrone. Because of its bone-building actions, small amounts of the estrone metabolite, 16α-OH estrone (which is produced by Phase I metabolism) are required by men. The adult male reference range is 3 – 11.4 μg/24 hr.
Estradiol (E2): Estradiol is produced from testosterone via aromatase. Estradiol is also readily converted to estrone via 17β-HSD, which is reversible. Small amounts are also produced in the adrenal cortex, adipose tissue, brain, arterial wall and, in males, in the testes. Unless converted to estrone, estradiol is metabolized into protective 2-OH estradiol (Phase I) and 2-methoxyestradiol ([2-CH3O estradiol], Phase II). The adult male reference range is 0.8 – 4.6 μg/24 hr.
Estriol (E3): Derived from estrone through the intermediate (bone-building but potentially oncogenic) 16α-OH estrone, estriol is the weakest estrogen with 20-30% less affinity for estrogen receptors. Also estriol stimulates ERβ and has anti-proliferative effects in estrogen sensitive prostatic tissues. The adult male reference range is 3.5 – 13.7 μg/24 hr.
Elevated total estrogens in men may be due to excessive testosterone supplementation (≥75 mg/day) or excessive aromatase activity, which is nearly always associated with insulin resistance.
If excessive aromatase activity is indicated, check for insulin resistance. The most accurate and definitive test for insulin resistance is the procedure published by Kraft.48
In addition to diet and exercise, supplementation with vitamin D,49, 50; chromium51,52, (most likely to be effective in insulin-resistant vs. insulin-sensitive patients and when combined with biotin53,54); and especially the natural plant extract berberine are very likely to be helpful.55, 56, 57, 58, 59, 60, 61, 62
Supplementation with Myomin (a combination of Chinese botanicals, 2 to 3 capsules BID63 and Chrysin (liposomal drops, 6 drops sublingually BID64,65 will also lessen aromatase activity; however, retest with 24-Hour Urine after 3 months to ensure sufficient 16α-OH estrone is present for bone health; run Serum Testosterone Metabolites to check 3β-adiol levels for protection against prostate cancer.
2/16α ratio: The ratio of 2-hydroxyestrone (2-OH E1) to 16α-hydroxyestrone (16α-OH E1) is one indicator of a man’s risk of developing prostate cancer. 2-OH E1, a Phase I metabolite of estrone, has weak estrogenic activity and is associated with protection against prostate cancer. 16α-OH E1, also a Phase I estrone metabolite, is an estrogen agonist, stimulates cell mitosis and proliferation, and is associated with increased risk of prostate cancer. However, 16α-OH estrone is also involved in bone building, so very low levels indicate increased risk for osteopenia/osteoporosis in men as well as women.66, 67, 68, 69, 70, 71, 72
The ideal 2/16α Ratio range is 2 to 4. A 2/16α Ratio of <2 indicates increased risk for prostate and laryngeal cancer. A 2/16α Ratio of >4 indicates increased risk for osteopenia, osteoporosis.
Fortunately, the 2/16α ratio is highly modifiable with natural interventions. Estrone’s conversion to (pro-carcinogenic) 16α-OH E1 is promoted by obesity, hypothyroidism, pesticides, alcohol and cimetidine. Conversion to (protective) 2-OH E1 is promoted by indole-3-carbinol (I3C), 3.3- diindoylmethane (DIM), flax, soy, omega-3 fatty acids and exercise. (I3C and DIM are phytochemicals in Brassica vegetables that induce CYP1A1, a Phase I enzyme that stimulates formation of 2-OH E1 while downregulating formation of 16α-OH E1. DIM forms spontaneously from dimerization of I3C in the presence of stomach acid and is thought to be the primary active agent in I3C.)73, 74, 75, 76, 77, 78, 79
Levels of 16a-OH E1 can also be lowered by increasing its conversion to estriol. This conversion is stimulated by iodine and iodide.80
Calcium D-glucarate supports proper estrogen excretion
The major route of estrogen elimination in humans is through Phase II glucuronidation (conjugation with glucuronic acid) in the liver. Glucose and inositol are oxidized in the liver to glucuronic acid and then bound into uridine diphosphate glucuronate (UDG), which is used by the enzyme uridine diphosphate transglucuronylase to convert 2-OH estrone, 4-OH estrone, 16α-OH estrone, estradiol or estriol into water-soluble glucuronides, which can be excreted through the urine as well as bile.
Calcium-D-glucarate is the calcium salt of D-glucaric acid. Oral supplementation with calcium-D-glucarate has been shown to inhibit beta-glucuronidase, an enzyme produced by colonic microflora (e.g., E.coli) that is capable of hydrolyzing glucuronide conjugates, thus returning estrogen readied for excretion back into circulation. Elevated beta-glucuronidase activity is associated with an increased risk for various cancers, particularly hormone-dependent cancers such as prostate, and colon cancers.81, 82
SEX HORMONES: PROGESTERONES
Progesterone: The major naturally occurring member of a class of structurally very similar hormones; in males, progesterone is produced by the brain.
Progesterone is an aromatase inhibitor,83 so may be useful for treating benign prostatic hyperplasia (BPH). Follow-up testing with the Serum Testosterone Metabolites assay is recommended to ensure over-inhibition of 5AR is not occurring.
Pregnanediol, an inactive progesterone metabolite, is used to provide an indirect (but accurate) measure of progesterone levels in the body since progesterone’s structure prevents it from being eliminated in urine in significant quantities.84, 85
In men, the Reference Range for pregnanediol is70-1050 μg/24hr.
SEX HORMONES: ANDROGENS
DHEA: produced in the adrenals, DHEA is the most abundant steroid in the human body. Levels peak between 25 to 30 years of age and then decline. After conversion into androstenedione, DHEA may be used to produce testosterone and its metabolites (for which reason DHEA replacement may help boost testosterone levels) or estrone, and thus 16α-OH estrone86.
For this reason, DHEA helps build new bone tissue and has been shown to significantly improve bone mineral density in older adults.87, 88, 89 Low levels are associated with increased risk of fracture and osteoporosis.90
DHEA and its metabolite etiocholanolone (also reported by the 24-Hour Urine Test, see below), inhibit glucose-6-phosphate dehydrogenase (G6PD), an enzyme that plays a key role in anerobic glycolysis, the major route of energy production for cancer cells.91, 92
DHEA has significant immune-modulatory functions—both immune-stimulatory and anti-glucocorticoid effects. Evidence is accumulating that DHEA may be effective as a treatment for the immunological abnormalities that arise in subjects with low circulating levels of this hormone, including the impaired immune response of older individuals and immune dysregulation in patients with chronic autoimmune disease.93
In men, as noted above, DHEA is a 5AR agonist, thus promoting conversion of testosterone to DHT, and has also been shown to exert anti-atherogenic effects; higher serum levels of DHEA-S correlate inversely with carotid artery intima-media thickness, plaque and blood flow volume.94
The Reference Range for DHEA is 100 – 2000 μg/24hr.
Etiocholanolone: One of two DHEA metabolites reported on the 24-Hour Urine Test, etiocholanolone, as noted above, has cancer-preventive anti-proliferative effects via its inhibition of G6PD. Etiocholanolone is produced from androstenedione by the enzyme 5β-reductase followed by 3α-hydroxysteroid dehydrogenase (3α-HSD). Excessive DHEA supplementation (>50 mg/day in males) may be the cause of high etiocholanolone levels.
The Reference Range for etiocholanolone is 500 – 5000 μg/24hr.
Androsterone: A DHEA metabolite derived from androstenedione via the activity of 5AR followed by 3α-hydroxysteroid dehydrogenase (3α-HSD), and therefore useful for monitoring 5AR. If androsterone is high in relation to etiocholanolone, 5AR activity may be elevated, resulting in increased conversion of testosterone to dihydrotestosterone (5α-DHT).
5α-DHT is ~3 times more powerful than testosterone and unlike testosterone, cannot be aromatized to estradiol. Thus, excess 5AR is associated with male pattern baldness. Excessive DHEA supplementation (>50 mg/day in males) is a possible cause of high androsterone levels. However, if androsterone is low in relation to etiocholanolone in men, then 5AR activity may be low as well, resulting in insufficient production of 3β-adiol (thus increasing prostate cancer risk) and leaving more testosterone to be aromatized to estradiol.
The Reference Range for androsterone is 2000 to 5000μg/24 hr in men.
Testosterone: Primarily secreted by the testes in men, but also produced in the adrenals, liver, skin and brain, testosterone is important not only for its effects on the male libido95,96, but on lean body mass and muscle strength, cardiovascular health, cognitive function and bone mineral density.97
The Reference Range for testosterone is 20 – 200μg/24 hr in men.
The range is wide because of the many different body types included in its calculation, which is based on 30+ years of 24 Hour Urine tests on thousands of men. Some men may produce less testosterone than other men and may have more active 5AR to compensate. For anti-aging, we generally recommend that, with treatment, men be between 80 – 150μg/24 hr. While some clinicians prefer to see testosterone levels in the upper end of the reference range to help with anti-aging, even though the patient could likely be symptom free with less HRT, we believe the key question is: “Is the testosterone dose sufficient to render the patient symptom-free?” In addition, hormones should always be evaluated comprehensively because of they constitute an interactive web. We can often get more benefit with less because when they are all balanced, they “cooperate” with each other. In terms of testosterone, if the patient is in the upper end of the reference range, it is essential to also run the Serum Testosterone Metabolite profile to check DHT and its metabolites.
5α-Androstanediol: On the 24 Hour Urine test, the 5α-androstanediol analyte contains both the 3α-adiol (aka 5α-Androstane-3α-17β-diol) and 3β-adiol (aka 5α-Androstane-3β-17β-diol) subcomponents, and does not differentiate between these final downstream metabolites of 5α-DHT. The 3α-adiol and 3β-adiol metabolites are able to be further differentiated and are reported on the Serum Testosterone Metabolite profile. 5α-Androstanediol is a testosterone/5α-DHT metabolite produced via the activity of 5AR. High levels indicate testosterone is primarily being metabolized through 5α-DHT, especially if levels of 5β-androstanediol are low. As noted above, 5α-DHT is highly potent: ~3 times more powerful than testosterone. Elevated 5AR activity may be linked to increased risk for male pattern baldness and benign prostatic hypertrophy. Over-inhibition of 5AR, however, has been linked to increased risk of aggressive prostate cancer. (As explained above, a Serum Testosterone Metabolite test will give you more insight into testosterone’s metabolization and potential over-inhibition.)
The Reference Range for 5α-Androstanediol in men is 22.0 – 131.0μg/24hr.
5β-Androstanediol: a testosterone/5β-DHT metabolite produced via the activity of 5β-reductase. High levels indicate testosterone is being metabolized through 5β-DHT, especially if levels of 5α-androstanediol are low. 5β-DHT is a weak testosterone metabolite.
The Reference Range for 5β-Androstanediol in men is 40.0 – 401.0μg/24hr.
GLUCOCORTICOIDS
Pregnanetriol: A progesterone metabolite and indicator of sufficient substrate for the cortisol pathway. The Reference Range for pregnanetriol is quite wide (200 – 1,500 μg/24hr). Mid-range is desirable.
Cortisol: After DHEA, cortisol is the second most plentiful steroid in a healthy person. Cortisol increases gluconeogenesis, affects protein and fat metabolism, and thyroid metabolism. (Both excess and insufficient cortisol inhibit, while normal levels promote the conversion of T4 to T3.)98, 99 Cortisol has potent immunosuppressive and anti-inflammatory activity.
In excess, however, cortisol promotes insulin resistance and many features of the metabolic syndrome (e.g., glucose intolerance, hypertension, dyslipidemia). High levels of cortisol also decrease the ability of osteoblasts to synthesize new bone and interfere with absorption of Ca2+ from the gastrointestinal tract.
In 21st century life, cortisol is often elevated due to unremitting stress and sleep deprivation, and in “Catch 22” fashion, elevated cortisol promotes both. Elevated cortisol (or cortisone, see below) is associated with Cushing disease, unipolar depression, sleep deprivation, anxiety, panic disorder, PTSD in its early stages, exogenous cortisol supplementation, high-dose licorice root supplementation, intense physical exercise, and acute ingestion of alcohol.
Clinical signs of adrenal excess include insomnia, anxiety, insulin resistance, obesity (especially truncal adiposity), hyperglycemia, hypertension, easy bruising in the extremities due to loss of subcutaneous adipose and connective tissue, bone loss, muscle weakness and sarcopenia. If causes are not addressed, adrenal fatigue and cortisol insufficiency is the likely outcome.
The Reference Range for cortisol is 30 – 170μg/24hr, which is quite wide and does not represent optimal levels. Optimal range for Cortisol is ~90μg/24hr.
Cortisone is the inactive metabolite of cortisol and serves as a “cortisol reserve,” in the body. Cortisone is produced by the action of 11β-hydroxysteroid dehydrogenase (11β-HSD), an enzyme with two isoforms, the first of which, 11β-hydroxysteroid dehydrogenase I (11β-HSD I) catalyzes cortisone into cortisol, enabling rapid supply of the active hormone as needed. The second isoform, 11β-HSD II, inactivates cortisol to cortisone (an action that is reversible via the activity of 11β-HSD I).
Decreased cortisol or cortisone seen with adrenal insufficiency is associated with Chronic Fatigue Syndrome, fibromyalgia, rheumatoid arthritis, and late stage Panic Disorder. Clinical signs of adrenal insufficiency include fatigue, exercise intolerance, hypoglycemia, salt craving, insomnia, depression, irritability, positive Hippus test (greater light exposure should result in pupil contraction), and low blood pressure.
The Reference Range for cortisone is 31 – 209μg/24 hr, which is quite wide and does not represent optimal levels. Optimal range for Cortisone is ~120-130μg/24hr.
Cortisol : Cortisone Ratio: The ideal cortisol : cortisone ratio is 0.7 (i.e., cortisone should be ~30% higher than cortisol), as this indicates slightly more storage (cortisone) than active (cortisol) hormone. Sleep problems are common when this ratio gets to ≥1.
A ratio greater than 1.4 is considered possibly suspicious for the hypertensive syndrome “Apparent Mineralocorticoid Excess Type 2” (AME Type 2 is a much milder version of AME Type 1, a severe and lethal congenital deficiency of 11β HSD II).
Tetrahydrocortisone, Tetrahydrocortisol, and Allo-tetrahydocortisol: are metabolites of cortisone (tetrahydrocortisone), and cortisol (tetrahydrocortisol, and allo-tetrahydocortisol), and can be used to determine daily cortisol output.
When their 24 Hour Urine Test values are added together, these three metabolites account for approximately half of daily cortisol output. Taking the sum of the three, doubling it and moving the decimal 3 points to the left will give, in milligrams, about how much cortisol is being made each day. In men, the three metabolites should add up to between 5,000 and 10,000, which corresponds to a cortisol output of 10-20 mg/day.
Low levels are a very strong indication of weak adrenal function. (If allo-tetrahydrocorticotsterone (5α-THB), tetrahydrocorticosterone (THB) and 11-dehydrotetrahydrocorticosterone (THA) levels are also low, this is a very strong indication of long term adrenal insufficiency. These analytes are discussed below.)
11β-OH Androsterone and 11β-OH Etiocholanolone: terminal metabolites of cortisol. Their values will confirm if cortisol production is excessive or insufficient. Often, as patients become insufficient, cortisol levels may still appear within normal range, but downstream metabolites will be low.
MINERALOCORTICOIDS
Aldosterone: The major mineralocorticoid, aldosterone is part of the renin-angiotensin system and acts on the distal tubules and collecting ducts of the nephron (the functional unit of the kidney) to cause conservation of sodium, secretion of potassium, increased water retention, and increased blood pressure. Aldosterone levels are usually a reliable indication of whether a person is on a normal, low or high salt diet.
Aldosterone reverses certain types of hearing loss inn experimental animals100, 101, 102, 103, and levels of serum aldosterone have been inversely correlated with degree of hearing in humans.104 Case studies at Tahoma Clinic, Renton, Washington, have found that a significant percentage of individuals with hearing loss and low levels of aldosterone recover some of their hearing when exogenous aldosterone is taken.105
(For further discussion and possible mitigating circumstances, see “Activity of 11β-Hydroxysteriod dehydrogenase I and II” below.) Reference ranges are: Normal Diet = 6.0 -25.0 μg/24hr; Low Salt = 17.0 -44.0μg/24hr; High Salt = 0.0 – 6.0μg/24hr.
Allo-tetrahydrocorticostersone (5α-THB), Tetrahydrocorticosterone (THB) and 11-dehydrotetrahyrdocorticosterone (THA): metabolites of aldosterone that serve as sensitive markers for monitoring acute adrenal stress. These metabolites are the first to rise in the ACTH stimulation test; high levels suggest acute stress at the time of collection. Low levels are a good indication of chronic adrenal fatigue. References ranges: 5α-THB = 130 – 600μg/24hr; THB = 30 – 240μg/24hr; THA = 62 – 293μg/24hr.
The most comprehensive 24-Hour Urine Test also reports levels of human Growth Hormone, free T3 and T4 (the thyroid hormones).
Human Growth Hormone: Produced in the anterior pituitary and regulated from hypothalamus by growth hormone releasing hormone and growth hormone inhibiting hormone (aka somatostatin), human growth hormone (hGH, aka somatotrophin) enters the circulation and is delivered to the liver where it is converted to growth factors that initiate muscle, bone, and cartilage production; improve kidney function, skin elasticity, and cell repair and regeneration. One thing growth hormone does not increase is body fat; hGH decreases adipose tissue.
IGF1, used to evaluate hGH levels in serum tests, is not considered a reliable marker106, 106; urine hGH is a better indicator.108, {ref109, 110, 111, 112
Growth hormone levels are increased by deep sleep,113 arginine (more effective in younger men, but useful in elders as well)114, 115, glutamine (helpful for older people, 2 grams at bedtime),116 and ornithine alpha-ketoglutarate (may boost the use of glutamine in arginine metabolism, 0.25 mg/kg)117, resistance training, short intense bursts of exercise, and vigorous aerobic exercise118, 4119, (although the effect of exercise is more pronounced in younger subjects)120, and adequate protein.121
A number of hormones increase hGH secretion including testosterone (the most potent secretagogue for hGH), estrogen, progesterone, thyroid, melatonin, and growth hormone releasing hormone (GHRH).122, 123, 124, 125 hGH is decreased by a sedentary lifestyle, inadequate protein, poor sleep, and insufficient endogenous hormones.
The adult Reference Range for hGH is 1065 – 4722μg/24hr. Mid-range is optimal.
Thyroid Hormones
Upon stimulation by thyroid-stimulating hormone (TSH), the thyroid produces two main hormones: thyroxine (T4), the major form of thyroid hormone in the blood, and triiodothyronine (T3), the active hormone (three to four times more potent than T4), which primarily regulates the metabolic machinery inside cells. (The ratio of T4 to T3 released into the blood is roughly 20 to 1.) Thyroid hormones’ effects include controlling the speed of protein synthesis, energy use, and sensitivity to other hormones.
Both thyroid hormones combine tyrosine with iodine (T4 with 4 iodine molecules, and T3 with 3 iodine molecules), thus iodine insufficiency prevents adequate thyroid hormone formation.
Even if TSH is effectively signaling the thyroid gland, and iodine is present in sufficient amounts for adequate production of T4 and T3 (blood test levels thus appearing normal), intra-cellular conversion to T3 may not occur for several reasons. T4 is converted to the T3 within cells by deiodinases (5′-iodinase), enzymes for which selenium is the required cofactor. Cortisol is also required for the conversion of T4 to T3; long-term stress, which depletes adrenal reserves of cortisone, will therefore cause inhibition of the T4 to T3 conversion. Inflammatory cytokines (notably interleukin-2) can promote formation of autoantibodies to the thyroid, again inhibiting the T4 to T3 conversion.126 Thus, a patient can have hypothyroid symptoms despite normal serum levels of thyroid hormones. The 24-Hour Urine test gives a better indication of what is happening inside the cell.127
Ideally, one wants to see higher levels of free T3 than free T4. The richest food source of selenium, Brazil nuts may help improve conversion of T4 to T3, and may also help lessen inflammation since selenium is a cofactor for reduction of glutathione peroxidases. One Brazil nut provides ~ 100 mcg of selenium; 200 mcg is the recommended dosage. Excessive selenium can interfere with enzyme systems related to sulfur metabolism and can be toxic in amounts greater than 900 mcg/day.128, 129, 130, 131
Urinary Minerals
Sodium: Reference range 40 – 220 mmol/24hr
Potassium: Reference range 25 – 150 mmol/24hr
Urinary levels of sodium and potassium clearly reflect dietary intake. The ideal ratio of sodium: potassium is 1.5. Due to the typical Western diet, which contains a disproportionate amount of high-sodium processed foods and few servings of potassium-rich green leafy and other vegetables, the ratio of sodium: potassium is typically elevated.
Bringing this ratio into ideal range is well recognized to be of vital importance in the prevention of hypertension, myocardial infarction, stroke and kidney failure.132, 133, 134, 135
When salt intake is high, even a modest reduction for a duration of 4 or more weeks has a significant and important beneficial effect on blood pressure in individuals with normal as well as elevated blood pressure. A modest and long-term reduction in population salt intake could significantly reduce strokes, heart attacks and heart failure.136 Decrease sodium by avoiding processed foods; increase potassium by increasing green leafy vegetable intake.
On the other hand, a 24 Hour Urine sodium on the low end of the reference range is not uncommon in people with low adrenal function. Many people have heard that it is beneficial to reduce salt and are over-zealous about it, and thus are not getting the sodium they require for good adrenal function.
Enzyme Activity
5α-Reductase is the enzyme that converts testosterone to the more potent 5α-DHT. Upregulated 5α-DHT activity promotes BPH and male pattern baldness, and is associated with insulin resistance and obesity.
5AR activity is reflected by two ratios on the 24-Hour Urine test:
(1) Androsterone/Etiocholanolone Ratio and (2) Allo-tetrahydrocortisol/tetrahydrocortisol Ratio.
If excessive, 5AR can be down-regulated by zinc137, 138, GLA,139 EPA,139 vitamin D3,140 saw palmetto141, progesterone142, 143, green tea extract144, finasteride, and dutasteride.
Over-inhibition of 5AR, however, can promote aggressive prostate cancer. In the Prostate Cancer Prevention Trial, a study involving more than 18,000 men, subjects taking dutasteride had a lower rate of prostate cancer, but a significantly higher rate of aggressive prostate cancers than the placebo group. This resulted in a higher absolute number of aggressive prostate cancers in the dutasteride group than in the placebo group – even though the placebo group had a higher rate of prostate cancer.145 (See above “Mechanisms through which 5α-reductase inhibitors promote prostate cancer”) (Neal, please make this a link to this section above) Thus, as we have seen elsewhere, e.g., rofecoxib (Vioxx®), celecoxib (Celebrex®), balance in biological processes is more beneficial than absolute interruption.)
11β-Hydroxysteriod dehydrogenase I and II are the enzymes that convert cortisone to cortisol and vice versa.
11β-Hydroxysteriod dehydrogenase I converts cortisone to cortisol. 11β Hydroysteroid dehydrogenase II converts cortisol to cortisone. 11β HSD I is inhibited by estradiol and HGH. 11β HSD II is inhibited by licorice and cadmium; this latter inhibition explains some of the hypertensive effects of these two substances.
11β-HSD I is highly expressed in key metabolic tissues including the liver, adipose tissue, and the central nervous system, where it reduces cortisone into the active hormone, cortisol.
11β-hydroxysteroid dehydrogenase II (11β-HSD II) is found in salivary glands and aldosterone-selective tissues, e.g. kidneys, where it oxidizes cortisol to cortisone to prevent activation of the mineralocorticoid receptor. As noted in Part I on this review, the presence of 11β-HSD II in salivary glands can invalidate salivary cortisol measurements.146
Activity of 11β-Hydroxysteriod dehydrogenase I and II is reflected by two ratios provided by the 24-Hour Urine Test:
(1) Cortisone: Cortisol Ratio
This ratio of hormone reserve (cortisone) to active hormone (cortisol) shows enzyme activity in adipose tissue and kidneys, and provides significant insight into the patient’s adrenal health. The ideal ratio is 0.7. Licorice, which contains glycyrrhetinic acid, can inhibit 11 β-HSD II, causing increased conversion of (storage) cortisone to (active) cortisol.
(2) Tetrahydrocortisol + allo-tetrathydrocortisol/Tetrahydrocortisone Ratio
Low ratios for these enzymes are associated with obesity and insulin resistance, while elevated ratios are associated with low-renin hypertension, high dose licorice, and exogenous cortisol. Ideal ratio is 0.9.
In patients with essential hypertension, elevated ratios may also be a sign of primary aldosteronism (PA), for which recent reports suggest incidence may be as high as 10-15% in hypertensive patients. PA may be missed in these patients because it can exist for many years before hypokalemia is demonstrable. Such patients are often mis-placed on anti-hypertensive medications, which do not prevent progression of the hypertensive vascular complications induced by hyperaldosteronemia (i.e., heart attack, stroke, kidney failure). If 11β-HSD ratios are elevated, hyperproduction of aldosterone will be detectable by ACTH-stimulated venous sampling.147
CONCLUSION
Serum and 24-Hour Urine Hormone Testing—Sine Qua Non for Optimal Men’s BHRT
Despite the brevity of this introductory overview of a very complex subject—how to safely and effectively monitor BHRT in your aging male patients—the necessity of assessing hormone metabolites has, hopefully, been demonstrated. By utilizing the latest serum Testosterone Metabolites tests in combination with the most comprehensive 24-Hour Urine tests, physicians can gain unprecedented insight into their male patients’ health, ensuring safe and effective BHRT.
Figure 2
| 24-Hour Urine Comprehensive Profile: Analytes & Reference Ranges for Men | ||
| Analyte | Adult Reference Range* | |
| Creatinine | 0.5 – 2.0 gm/24hr | |
| Total urine volume | 1,200 – 3,000 mL | |
| Steroid | Amount excreted in μg/24 hr | |
| Sex Hormones | ||
| Estrone (E1) | 3.0 – 11.4 | |
| Estradiol (E2) | 0.8 -4.6 | |
| Estriol (E3) | 3.5 – 13.7 | |
| Total Estrogens | 7.3 -29.7 | |
| 2-OH Estrone (Phase I metabolite) | 1.9 – 15.8 | |
| 16α-OH Estrone (Phase I metabolite) | 0.2 – 5.9 | |
| 2/16α Ratio (Ideal = 2 – 4) | 1.2 – 4.9 | |
| Pregnanediol (progesterone metabolite) | 70 – 1,050 | |
| DHEA | 100 – 2,000 | |
| Androsterone (DHEA metabolite) | 2,000 – 5,000 | |
| Etiocholanolone (DHEA metabolite) | 1,400 – 5,000 | |
| (Androsterone:etiocholanolone ratio, if low, suggestive of low 5AR activity, low 5α-DHT, low 3β-adiol) | ||
| Testosterone | 20 – 200 | |
| 5α-Androstanediol | 22 – 131 | |
| 5β-Androstanediol | 40 – 401 | |
| Glucocorticoids | ||
| Pregnanetriol ( want ≥mid-range, indicator of substrate availability for cortisol pathway ) | 200 – 1,500 | |
| Cortisone (optimal range ~120-130μg/24hr) | 31 – 209 | |
| Cortisol (optimal range ~90μg/24hr) | 30 – 170 | |
| Cortisone: Cortisol Ratio (always interconverting) | Ideal = 0.7 | |
| Tetrahydrocortisone (THE, cortisone metabolite) | 2,100 – 7,400 | |
| Allo-tetrahydrocortisol (5α-THF, cortisol metabolite) | 700 – 3,800 | |
| Tetrahydrocortisol (THF, cortisol metabolite) | 1,200 – 4,500 | |
| (THE + 5α-THF + THF) x2 = daily cortisol output | 8,000 – 10,000 | |
| 11β-OH Androsterone (terminal metabolite of cortisol; low value confirms insufficiency) | 613 – 2,298 | |
| 11β-OH Etiocholanolone (terminal metabolite of cortisol, low value confirms insufficiency) | 153 – 950 | |
| Mineralocorticoids | ||
| Aldosterone(indicator of salt level in diet, low may indicate adrenal fatigue) | Normal Diet = 6.0 – 25.0
Low Salt: 17.0 – 44.0 High Salt: 0.0 – 6.0 |
|
| Allo-tetrahydrocorticosterone (5α-THB, low = long term adrenal insufficiency, high = acute stress at collection) | 130 – 1600 | |
| Tetrahydrocorticosterone (THB, low = long term adrenal insufficiency, high = acute stress at collection) | 30 -240 | |
| 11-dehydrotetrahydrocorticosterone (THA, low = long term adrenal insufficiency, high = acute stress at collection) | 76 – 456 | |
| Human Growth Hormone | 1,065 – 4,722 | |
| Thyroid Hormones | ||
| Free T3 | 470 – 1,750 | |
| Free T4 | 430 -3,200 | |
| T3 + T4 (if <1000 adrenal support may be indicated) | ~1000 | |
| Urinary Sodium and Potassium | ||
| Sodium | 40 – 220 | |
| Potassium | 25 – 150 | |
| Sodium:Potassium Ratio (ideal 1.5, if low consider malabsorption) | 1.2 – 4.8 | |
| Enzyme Activity | ||
| 5α-Reductase enzyme (converts testosterone to more potent 5α-DHT) activity as shown by: | ||
| Androsterone/Etiocholanolone Ratio | Ideal = Mid-range 0.7 | |
| Allo-tetrahydrocortisol /Tetrahydrocortisol Ratio | Ideal = Mid-range 0.6 | |
| Elevated 5AR activity associated BPH, premature baldness, obesity, insulin resistance in men
Low 5AR activity suggestive of reduced conversion of testosterone to DHT, undervirilization, low 3β-adiol production, increased prostate cancer risk |
||
| 11β-Hydroxysteriod dehydrogenase I and II (isoforms of enzyme that converts cortisol to cortisone) activity shown by: | ||
| Cortisol: Cortisone Ratio | Ideal 0.7 | |
| Tetrahydrocortisol + allo-tetrahydrocortisol: Tetrahyrdocortisone Ratio | Ideal 0.9 | |
| Low ratios associated w/obesity & insulin resistance. Elevated ratios w/low-renin hypertension, high dose licorice, exogenous cortisol. | ||
| *Reference ranges vary by lab and can may be expressed in different units of measure | ||
References
- Burtis CA, Ashwood ER.. Tietz Textbook of Clinical Chemistry 3rd Edition.. W.B. Saunders Company: Philadelphia, PA, 1999, Function of Adrenal Cortex, p1530-1569; Reproductive Endocrine Function, p1601-1641.. ↑
- Raffaelli A, Saba A, Vignali E, Marcocci C, et al.. Direct determination of the ratio of tetrahydrocortisol+allo-tetrahydrocortisol to tetrahydrocortisone in urine by LC-MS-MS.. J Chromatogr B Analyt Technol Biomed Life Sci. . 2006 Jan 18;830(2):278-85.. ↑
Abstract - Yazici M, Sahin M, Bolu E, et al. . Prediction of testosterone response to human chorionic gonadotrophin in idiopathic hypogonadotropic hypogonadism patients.. J Natl Med Assoc.. 2009 Jan;101(1):71-6. PMID: 19245075. ↑
Abstract - Amory JK, Coviello AD, Page ST, et al. . Serum 17-hydroxyprogesterone strongly correlates with intratesticular testosterone in gonadotropin-suppressed normal men receiving various dosages of human chorionic gonadotropin. . Fertil Steril . 89: 380–386, 2008. PMID: 17462643. ↑
Abstract - Kushnir MM, Rockwood AL, Bergquist J. . Liquid chromatography-tandem mass spectrometry applications in endocrinology. . Mass Spectrom Rev. . 2010 May-Jun;29(3):480-502. PMID: 19708015. ↑
Abstract - Rauh M.. Steroid measurement with LC-MS/MS. Application examples in pediatrics.. J Steroid Biochem Mol Biol.. 2010 Aug;121(3-5):520-7. Epub 2009 Dec 28. PMID: 20036331. ↑
Abstract - Cuningham GR, Toma SM. . Why is androgen replacement in males controversial? . J Clin Endocrinol Metab.. 2011 Jan;96(1):38-52. PMID: 20881265. ↑
Abstract - Bhasin S, Cunningham GR, Hayes FJ, et al. . Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. . J Clin Endocrinol Metab. . 2010 Jun;95(6):2536-59. PMID: 20525905. ↑
Abstract - Wang C, Cunningham G, Dobs A, et al. . Long-term testosterone gel (AndroGel) treatment maintains beneficial effects on sexual function and mood, lean and fat mass, and bone mineral density in hypogonadal men.. J Clin Endocrinol Metab.. 2004 May;89(5):2085-98. PMID: 15126525. ↑
Abstract - Wang C, Harnett M, Dobs AS, Swerdloff RS. . Pharmacokinetics and safety of long-acting testosterone undecanoate injections in hypogonadal men: an 84-week phase III clinical trial.. J Androl. . 2010 Sep-Oct;31(5):457-65. Epub 2010 Feb 4. PMID: 20133964. ↑
Abstract - Jockenhövel F. . Testosterone therapy–what, when and to whom? . Aging Male.. 2004 Dec;7(4):319-24. PMID: 15799128. ↑
Abstract - Barba M, Yang L, Schünemann HJ, Sperati F, et al.. Urinary estrogen metabolites and prostate cancer: a case-control study and meta-analysis.. J Exp Clin Cancer Res. . 2009 Oct 8;28:135. PMID: 19814782. ↑
Abstract - Lyon M, Bland J, Jones D. . Chapter 31: Clinical Approaches to Detoxification and Biotransformation . Textbook of Functional Medicine, . Institute for Functional Medicine, Gig Harbor, WA, 2005, p. 564.. ↑
- Maggio M, Lauretani F, Basaria S, et al. . Sex hormone binding globulin levels across the adult lifespan in women–the role of body mass index and fasting insulin.. J Endocrinol Invest.. 2008 Jul;31(7):597-601 PMID: 18787375 . ↑
Abstract - Wright AS, Douglas RC, Thomas LN, et al. . Androgen-induced regrowth in the castrated rat ventral prostate: role of 5alpha-reductase.. Endocrinology.. 1999 Oct;140(10):4509-15. PMID: 10499505. ↑
Abstract - Nishiyama T, Ikarashi T, Hashimoto Y,et al. . Association between the dihydrotestosterone level in the prostate and prostate cancer aggressiveness using the Gleason score.. J Urol.. 2006 Oct;176(4 Pt 1):1. ↑
Abstract - Kjellman A, Akre O, Norming U, et al. . Dihydrotestosterone levels and survival in screening-detected prostate cancer: a 15-yr follow-up study.. Eur Urol. . 2008 Jan;53(1):106-11. Epub 2007 Apr 26. PMID: 17482753. ↑
Abstract - Hoffman RM, Roberts RG, Barry MJ. . Battling Prostate Cancer with 5-Alpha-Reductase Inhibitors: a Pyrrhic Victory? . J Gen Intern Med. . 2011 Jan 11. [Epub ahead of print] PMID: 21222171. ↑
Abstract - Eikenberry SE, Nagy JD, Kuang Y. . The evolutionary impact of androgen levels on prostate cancer in a multi-scale mathematical model.. Biol Direct. . 2010 Apr 20;5:24. PMID: 20406442. ↑
Abstract - Nishiyama T, Ikarashi T, Hashimoto Y, et al.. The change in the dihydrotestosterone level in the prostate before and after androgen deprivation therapy in connection with prostate cancer aggressiveness using the Gleason score. . J Urol.. 2007 Oct;178(4 Pt 1):1282-8; discussion 1288-9. Epub 2007 Aug 14. PMID: 17698092. ↑
Abstract - Kramer BS, Hagerty KL, Justman S, et al. . Use of 5-alpha-reductase inhibitors for prostate cancer chemoprevention: American Society of Clinical Oncology/American Urological Association 2008 Clinical Practice Guideline. J Clin Oncol. . 2009 Mar 20;27(9):1502-16. Epub 2009 Feb 24. PMID: 19252137. ↑
Abstract - Dondi D, Piccolella M, Biserni A, et al.. Estrogen receptor beta and the progression of prostate cancer: role of 5alpha-androstane-3beta,17beta-diol.. Endocr Relat Cancer.. 2010 Jul 28;17(3):731-42. Pri. ↑
Abstract - Oliveira AG, Coelho PH, Guedes FD, et al. . 5alpha-Androstane-3beta,17beta-diol (3beta-diol), an estrogenic metabolite of 5alpha-dihydrotestosterone, is a potent modulator of estrogen receptor ERbeta expression in the ventral prostrate of adult. Steroids. . 2007 Dec;72(14):914-22. Epub 2007 Aug 9. PMID: 17854852. ↑
Abstract - Guerini V, Sau D, Scaccianoce E, et al. . The androgen derivative 5alpha-androstane-3beta,17beta-diol inhibits prostate cancer cell migration through activation of the estrogen receptor beta subtype. . Cancer Res.. 2005 Jun 15;65(12):5445-53. PMID: 15958594. ↑
Abstract - Handa RJ, Weiser MJ, Zuloaga DG. . A role for the androgen metabolite, 5alpha-androstane-3beta,17beta-diol, in modulating oestrogen receptor beta-mediated regulation of hormonal stress reactivity. . J Neuroendocrinol. . 2009 Mar;21(4):351-8. PMID: 19207807. ↑
Abstract - Bao AM, Meynen G, Swaab DF. . The stress system in depression and neurodegeneration: focus on the human hypothalamus. . Brain Res Rev. 2008 Mar;57(2):531-53. Epub 2007 Apr 27. PMID: 17524488. ↑
Abstract - We are currently aware of only one compounding pharmacy that is a source 3β-Adiol. . —Madison Pharmacy Associates, 1289 Deming Way, Madison, WI 53717-2007, (608)-833-7046, . Hopefully, others will soon follow suit.. ↑
- Abe M, Ito Y, Oyunzul L, et al. . Pharmacologically relevant receptor binding characteristics and 5alpha-reductase inhibitory activity of free Fatty acids contained in saw palmetto extract. . Biol Pharm Bull.. 2009 Apr;32(4):646-50. PMID: 19336899. ↑
Abstract - Pham H, Ziboh VA. . 5 alpha-reductase-catalyzed conversion of testosterone to dihydrotestosterone is increased in prostatic adenocarcinoma cells: suppression by 15-lipoxygenase metabolites of gamma-linolenic & eicosapent. J Steroid Biochem Mol Biol. . 2002 Nov;82(4-5):393-400. PMID: 12589947. ↑
Abstract - Liu J, Shimizu K, Kondo R. . Anti-androgenic activity of fatty acids. . Chem Biodivers.. 2009 Apr;6(4):503-12. PMID: 19353546. ↑
Abstract - Bratoeff E, Segura T, Recillas S, et al. . Aromatic esters of progesterone as 5alpha-reductase and prostate growth inhibitors.. J Enzyme Inhib Med Chem.. 2009 Jun;24(3):655-62. PMID: 18825535; . ↑
Abstract - Hess-Wilson JK, Knudsen KE. . Endocrine disrupting compounds and prostate cancer. . Cancer Lett. . 2006 Sep 8;241(1):1-12. Epub 2005 Nov 17. PMID: 16298040. ↑
Abstract - Prins GS. . Endocrine disruptors and prostate cancer risk.. Endocr Relat Cancer.. 2008 Sep;15(3):649-56. Epub 2008 Jun 4. PMID: 18524946. ↑
Abstract - Lakshman KM, Kaplan B, Travison TG, et al. . The effects of injected testosterone dose and age on the conversion of testosterone to estradiol and dihydrotestosterone in young and older men. . J Clin Endocrinol Metab.. 2010 Aug;95(8):3955-64. Epub 2010 Jun 9. PMID: 20534765. ↑
Abstract - Luu-The V, Bélanger A, Labrie F. . Androgen biosynthetic pathways in the human prostate.. Best Pract Res Clin Endocrinol Metab.. 2008 Apr;22(2):207-21. PMID: 18471780. ↑
Abstract - Aizawa K, Iemitsu M, Maeda S, et al. . Acute exercise activates local bioactive androgen metabolism in skeletal muscle.. Steroids.. 2010 Mar;75(3):219-23. Epub 2010 Jan 4. PMID: 20045012. ↑
Abstract - Parsons JK, Palazzi-Churas K, Bergstrom J, et al. . Prospective study of serum dihydrotestosterone and subsequent risk of benign prostatic hyperplasia in community dwelling men: the Rancho Bernardo Study.. J Urol. . 2010 Sep;184(3):1040-4. PMID: 20643424. ↑
Abstract - Trifiro MD, Parsons JK, Palazzi-Churas K, et al.. Serum sex hormones and the 20-year risk of lower urinary tract symptoms in community-dwelling older men.. BJU Int. . 2010 Jun;105(11):1554-9. Epub 2009 Dec 7. PMID: 20002438. ↑
Abstract - Gustafsson O, Norming U, Gustafsson S, et al. . Dihydrotestosterone and testosterone levels in men screened for prostate cancer: a study of a randomized population. . Br J Urol. . 1996 Mar;77(3):433-40. PMI. ↑
Abstract - Gooren LJ, Saad F, Haide A, et al. . Decline of plasma 5alpha-dihydrotestosterone (DHT) levels upon testosterone administration to elderly men with subnormal plasma testosterone and high DHT levels. . Andrologia. 8811920. 2008 Oct;40(5):298-302. PMID: 18811920. ↑
Abstract - Lephart ED, Simpson ER, Trzeciak WH. . Rat adrenal 5 alpha-reductase mRNA content and enzyme activity are sex hormone dependent.. J Mol Endocrinol. . 1991 Apr;6(2):163-70. PMID: 2043243. ↑
Abstract - Yang Q, Titus MA, Fung KM, et al. . 5alpha-androstane-3alpha,17beta-diol supports human prostate cancer cell survival and proliferation through androgen receptor-independent signaling pathways: implication of androgen-independent prosta. J Cell Biochem. . 2008 Aug 1;104(5):1612-24. PMID: 18320593. ↑
Abstract - Eliassen AH, Ziegler RG, Rosner B, et al.. Reproducibility of fifteen urinary estrogens and estrogen metabolites over a 2- to 3-year period in premenopausal women.. Cancer Epidemiol Biomarkers Prev. . 2009 Nov;18(11):2860-8. Epub 2009 Oct 20. PMID: 19843676. ↑
Abstract - Falk RT, Xu X, Keefer L, et al. . A liquid chromatography-mass spectrometry method for the simultaneous measurement of 15 urinary estrogens and estrogen metabolites: assay reproducibility and interindividual variability. . Cancer Epidemiol Biomarkers Prev. . 2008 Dec;17(12):3411-8. PMID: 19064556. ↑
Abstract - Faupel-Badger JM, Fuhrman BJ, Xu X, et al. . Comparison of liquid chromatography-tandem mass spectrometry, RIA, and ELISA methods for measurement of urinary estrogens. . Cancer Epidemiol Biomarkers Prev.. 2010 Jan;19(1):292-300. PMID: 20056650. ↑
Abstract - Wolthers BG, Kraan GP. . Clinical applications of gas chromatography and gas chromatography-mass spectrometry of steroids.. J Chromatogr A. . 1999 May 28;843(1-2):247-74. PMID: 10399855. ↑
Abstract - Moon JY, Jung HJ, Moon MH, et al.. Heat-map visualization of gas chromatography-mass spectrometry based quantitative signatures on steroid metabolism.. J Am Soc Mass Spectrom. . 2009 Sep;20(9):1626-37. PMID: 19497759. ↑
Abstract - Kraft JR, Wehrmacher WH. . Diabetes–a silent disorder. . Compr Ther. . 2009 Fall-Winter;35(3-4):155-9. PMID: 20043611; . ↑
Abstract - Frost M, Abrahamsen B, Nielsen TL, et al.. Vitamin D status and PTH in young men: a cross-sectional study on associations with bone mineral density, body composition and glucose metabolism. . Clin Endocrinol (Oxf). . 2010 Nov;73(5):573-80. doi: 10.1111/j.1365-2265.2010.03847.x. PMID: 20718769. ↑
Abstract - Kayaniyil S, Vieth R, Harris SB, et al. . Association of 25(OH)D and PTH with metabolic syndrome and its traditional and nontraditional components. . J Clin Endocrinol Metab. . 2011 Jan;96(1):168-75. Epub 2010 Oct 27. PMID: 20980431. ↑
Abstract - Davì G, Santilli F, Patrono C.. Nutraceuticals in diabetes and metabolic syndrome.. Cardiovasc Ther. . 2010 Aug;28(4):216-26. Review. PMID:20633024. ↑
Abstract - Wang ZQ, Qin J, Martin J, et al.. Phenotype of subjects with type 2 diabetes mellitus may determine clinical response to chromium supplementation. . Metabolism.. 2007 Dec;56(12):1652-5. PMID: 17998017 . ↑
Abstract - Geohas J, Daly A, Juturu V, et al. . Chromium picolinate and biotin combination reduces atherogenic index of plasma in patients with type 2 diabetes mellitus: a placebo-controlled, double-blinded, randomized clinical trial. . Am J Med Sci. . 2007 Mar;333(3):145-53. PMID: 17496732. ↑
Abstract - Albarracin CA, Fuqua BC, Evans JL, et al.. Chromium picolinate and biotin combination improves glucose metabolism in treated, uncontrolled overweight to obese patients with type 2 diabetes. . Diabetes Metab Res Rev.. 2008 Jan-Feb;24(1):41-51. PMID: 17506119. ↑
Abstract - Yin J, Xing H, Ye J. . Efficacy of berberine in patients with type 2 diabetes mellitus. . Metabolism.. 2008 May;57(5):712-7. PMID: 18442638. ↑
Abstract - Zhang Y, Li X, Zou D, et al.. Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. . J Clin Endocrinol Metab.. 2008 Jul;93(7):2559-65. Epub 2008 Apr 8. PMID: 18397984. ↑
Abstract - Turner N, Li JY, Gosby A, et al. . Berberine and its more biologically available derivative, dihydroberberine, inhibit mitochondrial respiratory complex I: a mechanism for the action of berberine to activate AMP-activated protein kinas. Diabetes. . 2008 May;57(5):1414-8. Epub 2008 Feb 19. PMID: 18285556. ↑
Abstract - Zhang H, Wei J, Xue R, et al. . Berberine lowers blood glucose in type 2 diabetes mellitus patients through increasing insulin receptor expression. . Metabolism. . 2010 Feb;59(2):285-92. Epub 2009 Oct 1. PMID: 19800084. ↑
Abstract - Kong WJ, Zhang H, Song DQ, et al.. Berberine reduces insulin resistance through protein kinase C-dependent up-regulation of insulin receptor expression. . Metabolism. . 2009 Jan;58(1):109-19. PMID: 19059538. ↑
Abstract - Chen C, Zhang Y, Huang C.. Berberine inhibits PTP1B activity and mimics insulin action. . Biochem Biophys Res Commun. . 2010 Jul 2;397(3):543-7. Epub 2010 May 31. PMID: 20515652. ↑
Abstract - Yu Y, Liu L, Wang X, et al. . Modulation of glucagon-like peptide-1 release by berberine: in vivo and in vitro studies. . Biochem Pharmacol.. 2010 Apr 1;79(7):1000-6. Epub 2009 Nov 27. PMID: 19945441. ↑
Abstract - Al-masri IM, Mohammad MK, Tahaa MO. . Inhibition of dipeptidyl peptidase IV (DPP IV) is one of the mechanisms explaining the hypoglycemic effect of berberine. . J Enzyme Inhib Med Chem. . 2009 Oct;24(5):1061-6. PMID: 19640223. ↑
Abstract - Chi T.. Myomin: a natural aromatase inhibitor for estrogen-related conditions. . Townsend Letter, . Dec 2009 @ . ↑
http://findarticles.com/p/articles/mi_7396/is_317/ai_n45060728/) - Edmunds KM, Holloway AC, Crankshaw DJ, et al. . The effects of dietary phytoestrogens on aromatase activity in human endometrial stromal cells. Reprod Nutr Dev.. 2005 Nov-Dec;45(6):709-20. PMID: 16285913 . ↑
Abstract - Séralini G, Moslemi S. . Aromatase inhibitors: past, present and future. . Mol Cell Endocrinol. . 2001 Jun 10;178(1-2):117-31. PMID: 11403901; . ↑
Abstract - Bradlow HL, Telang NT, Sepkovic DW, et al. . 2-hydroxyestrone: the ‘good’ estrogen. . J Endocrinol. . 1996 Sep;150 Suppl:S259-65. PMID: 8943806 . ↑
Abstract - Sepkovic DW, Bradlow HL. . Estrogen hydroxylation–the good and the bad. . Ann N Y Acad Sci. . 2009 Feb;1155:57-67. PMID: 19250192. ↑
Abstract - Barba M, Yang L, Schünemann HJ, et al. . Urinary estrogen metabolites and prostate cancer: a case-control study and meta-analysis. . J Exp Clin Cancer Res.. 2009 Oct 8;28:135. PMID: 19814782. ↑
Abstract - Kabat GC, O’Leary ES, Gammon MD, et al.. Estrogen metabolism and breast cancer. . Epidemiology. . 2006 Jan;17(1):80-8. PMID: 16357599. ↑
Abstract - Robinson JA, Waters KM, Turner RT, et al. . Direct action of naturally occurring estrogen metabolites on human osteoblastic cells. . J Bone Miner Res. . 2000 Mar;15(3):499-506. PMID: 10750564. ↑
Abstract - Lotinun S, Westerlind KC, Kennedy AM, et al. . Comparative effects of long-term continuous release of 16 alpha-hydroxyestrone and 17 beta-estradiol on bone, uterus, and serum cholesterol in ovariectomized adult rats. . Bone. . 2003 Jul;33(1):124-31. PMID: 12919707. ↑
Abstract - Napoli N, Faccio R, Shrestha V, et al. . Estrogen metabolism modulates bone density in men. . Calcif Tissue Int. . 2007 Apr;80(4):227-32. Epub 2007 Apr 4. PMID: 17406768. ↑
Abstract - Bradlow HL, Zeligs MA.. Diindolylmethane (DIM) spontaneously forms from indole-3-carbinol (I3C) during cell culture experiments. . In Vivo.. 2010 Jul-Aug;24(4):387-91. PMID: 20668304. ↑
Abstract - Lord RS, Bongiovanni B, Bralley JA. . Estrogen metabolism and the diet-cancer connection: rationale for assessing the ratio of urinary hydroxylated estrogen metabolites. . Altern Med Rev. . 2002 Apr;7(2):112-29. PMID: 11991791. ↑
Abstract - Higdon JV, Delage B, Williams DE, et al.. Cruciferous vegetables and human cancer risk: epidemiologic evidence and mechanistic basis. . Pharmacol Res. . 2007 Mar;55(3):224-36. Epub 2007 Jan 25. PMID: 17317210. ↑
Abstract - Fowke JH, Longcope C, Hebert JR. . Brassica vegetable consumption shifts estrogen metabolism in healthy postmenopausal women. . Cancer Epidemiol Biomarkers Prev. . 2000 Aug;9(8):773-9. PMID: 10952093 . ↑
Abstract - Xu X, Duncan AM, Wangen KE, et al. . Soy consumption alters endogenous estrogen metabolism in postmenopausal women. . Cancer Epidemiol Biomarkers Prev. . 2000 Aug;9(8):781-6. PMID: 10952094. ↑
Abstract - Sturgeon SR, Volpe SL, Puleo E, et al. . Effect of flaxseed consumption on urinary levels of estrogen metabolites in postmenopausal women. . Nutr Cancer. . 2010;62(2):175-80. PMID: 20099191. ↑
Abstract - Bentz AT, Schneider CM, Westerlind KC. . The relationship between physical activity and 2-hydroxyestrone, 16alpha-hydroxyestrone, and the 2/16 ratio in premenopausal women (United States). . Cancer Causes Control. . 2005 May;16(4):455-61. PMID: 15953988. ↑
Abstract - Wright JV.. Bio-identical steroid hormone replacement: selected observations from 23 years of clinical and laboratory practice. . Ann N Y Acad Sci. . 2005 Dec;1057:506-24. PMID: 16399916. ↑
Abstract - [No authors listed]. Calcium-D-glucarate.. Altern Med Rev. . 2002 Aug;7(4):336-9. PMID: 12197785;. ↑
Abstract - Zółtaszek R, Hanausek M, Kiliańska ZM, et al.. [The biological role of D-glucaric acid and its derivatives: potential use in medicine] . Postepy Hig Med Dosw (Online). . 2008 Sep 5;62:451-62. PMID: 18772850. ↑
Abstract - Shimizu Y, Mita S, Takeuchi T, et al . Dienogest, a synthetic progestin, inhibits prostaglandin E(2) production and aromatase expression by human endometrial epithelial cells in a spheroid culture system. . Steroids.. 2010 Sep 21. [Epub ahead of print] PMID: 20851710. ↑
Abstract - Fabres C, Zegers-Hochschild F, Altieri E, et al.. Validation of the dual analyte assay of the oestrone:pregnanediol ratio in monitoring ovarian function. . Hum Reprod. . 1993 Feb;8(2):208-10 PMID: 8473420. ↑
Abstract - Collins WP, Collins PO, Kilpatrick MJ, et al. . The concentrations of urinary oestrone-3-glucuronide, LH and pregnanediol-3alpha-glucuronide as indices of ovarian function. Acta Endocrinol (Copenh).. 1979 Feb;90(2):336-48. PMID: 419920. ↑
Abstract - Labrie F, Luu-The V, Labrie C, et al. . DHEA and its transformation into androgens and estrogens in peripheral target tissues: intracrinology. . Front Neuroendocrinol. . 2001 Jul;22(3):185-212. PMID: 11456468 . ↑
Abstract - Jankowski CM, Gozansky WS, Kittelson JM, et al. Increases in bone mineral density in response to oral dehydroepiandrosterone replacement in older adults appear to be mediated by serum estrogens. . J Clin Endocrinol Metab. . 2008 Dec;93(12):4767-73. Epub 2008 Sep 23. PMID: 18812486. ↑
Abstract - von Mühlen D, Laughlin GA, Kritz-Silverstein D, et al. . Effect of dehydroepiandrosterone supplementation on bone mineral density, bone markers, and body composition in older adults: the DAWN trial. . Osteoporos Int. . 2008 May;19(5):699-707. Epub 2007 Dec 15. PMID: 18084691. ↑
Abstract - Weiss EP, Shah K, Fontana L, et al. . Dehydroepiandrosterone replacement therapy in older adults: 1- and 2-y effects on bone. . Am J Clin Nutr.. 2009 May;89(5):1459-67. Epub 2009 Mar 25. PMID: 19321570. ↑
Abstract - Garnero P, Sornay-Rendu E, Claustrat B, et al. . Biochemical markers of bone turnover, endogenous hormones and the risk of fractures in postmenopausal women: the OFELY study. . J Bone Miner Res.. 2000 Aug;15(8):1526-36. PMID: 10934651. ↑
Abstract - Yoshida S, Honda A, Matsuzaki Y, et al. . Anti-proliferative action of endogenous dehydroepiandrosterone metabolites on human cancer cell lines. . Steroids.. 2003 Jan;68(1):73-83.PMID: 12475725. ↑
Abstract - Matsuzaki Y, Honda A. . Dehydroepiandrosterone and its derivatives: potentially novel anti-proliferative and chemopreventive agents. . Curr Pharm Des.. 2006;12(26):3411-21. PMID: 17017935. ↑
Abstract - Hazeldine J, Arlt W, Lord JM.. Dehydroepiandrosterone as a regulator of immune cell function. . J Steroid Biochem Mol Biol. . 2010 May 31;120(2-3):127-36. Epub 2010 Jan 12. PMID: 20060904. ↑
Abstract - Yoshida S, Aihara K, Azuma H, et al. . Dehydroepiandrosterone sulfate is inversely associated with sex-dependent diverse carotid atherosclerosis regardless of endothelial function. . Atherosclerosis.. 2010 Sep;212(1):310-5. Epub 2010 Jun 2. PMID: 20627295. ↑
Abstract - Kingsberg SA, Simon JA, Goldstein I., et al. . The current outlook for testosterone in the management of hypoactive sexual desire disorder in postmenopausal women. . J Sex Med.. 2008 Sep 2;5 Suppl 4:182-93; quiz 193. PMID: 18783534. ↑
Abstract - Kingsberg S. . Testosterone treatment for hypoactive sexual desire disorder in postmenopausal women. . J Sex Med. . 2007 Mar;4 Suppl 3:227-34. PMID: 17394595. ↑
Abstract - van Geel TA, Geusens PP, Winkens B, et al. . Measures of bioavailable serum testosterone and estradiol and their relationships with muscle mass, muscle strength and bone mineral density in postmenopausal women: a cross-sectional study. . Eur J Endocrinol. . 2009 Apr;160(4):681-7. Epub 2009 Jan 27. PMID: 19174532. ↑
Abstract - Kelly GS. . Peripheral metabolism of thyroid hormones: a review. . Altern Med Rev. . 2000 Aug;5(4):306-33. PMID: 10956378. ↑
Abstract - Pizzorno L, Ferril W. “. “Thyroid,” in Clinical Approaches to Hormonal and Neuroendocrine Imbalances, Chapter 32, . Textbook of Functional Medicine, . Institute of Functional Medicine, Gig Harbor, WA, 2005, p.645.. ↑
- Trune DR, Kempton JB, Gross ND. . Mineralocorticoid receptor mediates glucocorticoid treatment effects in the autoimmune mouse ear. . Hear Res. . 2006 Feb;212(1-2):22-32. Epub 2005 Nov 22. PMID: 16307853. ↑
Abstract - Trune DR, Kempton JB. . Aldosterone and prednisolone control of cochlear function in MRL/MpJ-Fas(lpr) autoimmune mice. . Hear Res. . 2001 May;155(1-2):9-20. PMID: 11335072. ↑
Abstract - Trune DR, Kempton JB, Kessi M.. Aldosterone (mineralocorticoid) equivalent to prednisolone (glucocorticoid) in reversing hearing loss in MRL/MpJ-Fas1pr autoimmune mice. . Laryngoscope. . 2000 Nov;110(11):1902-6. PMID: 11081607. ↑
Abstract - Gross ND, Kempton JB, Trune DR.. Spironolactone blocks glucocorticoid-mediated hearing preservation in autoimmune mice. . Laryngoscope.. 2002 Feb;112(2):298-303. PMID: 11889387. ↑
Abstract - Tadros SF, Frisina ST, Mapes F, et al. . Higher serum aldosterone correlates with lower hearing thresholds: a possible protective hormone against presbycusis. . Hear Res.. 2005 Nov;209(1-2):10-8. Epub 2005 Jul 20. PMID: 16039078. ↑
Abstract - Wright JV, Russel L.. Nutrition & Healing Newsletter. January 2011. . ↑
http://wrightnewsletter.com/2010/01/01/january-2011/ - Corneli G, Gasco V, Prodam F, et al.. Growth hormone levels in the diagnosis of growth hormone deficiency in adulthood. . Pituitary.. 2007;10(2):141-9. PMID: 17429591. ↑
Abstract - Gasco V, Corneli G, Rovere S, et al.. Diagnosis of adult GH deficiency.. Pituitary. . 2008;11(2):121-8. PMID: 18404387. ↑
Abstract - Butt DA, Sochett EB.. Urinary growth hormone: a screening test for growth hormone sufficiency. . Clin Endocrinol (Oxf). . 1997 Oct;47(4):447-54. PMID: 9404443 . ↑
Abstract - Audí L, Antonia Llopis M, Luisa Granada M, et al. . [Low sensitivity of IGF-I, IGFBP-3 and urinary GH in the diagnosis of growth hormone insufficiency in slowly-growing short-statured boys. . Grupo Español de Estudio de la Talla Baja. Med Clin (Barc).. 2001 Jan 13;116(1):6-11. PMID: 11181253. ↑
Abstract - Bates AS, Evans AJ, Jones P, et al. . Assessment of GH status in adults with GH deficiency using serum growth hormone, serum insulin-like growth factor-I and urinary growth hormone excretion. . Clin Endocrinol (Oxf). . 1995 Apr;42(4):425-30. PMID: 7750197. ↑
Abstract - Kubota A, Ogawa H, Igarashi Y, et al. . Screening for growth hormone deficiency using urinary growth hormone measurement. . Acta Paediatr Jpn. . 1993 Oct;35(5):373-6. PMID: 8256618. ↑
Abstract - Walker JM, Wood PJ, Williamson S, et al. Urinary . Urinary growth hormone excretion as a screening test for growth hormone deficiency. . Arch Dis Child. . 1990 Jan;65(1):89-92. PMID: 2301989 . ↑
Abstract - Van Cauter E, Latta F, Nedeltcheva A, et al. . Reciprocal interactions between the GH axis and sleep. . Growth Horm IGF Res.. 2004 Jun;14 Suppl A:S10-7.PMID: 15135771. ↑
Abstract - Heffernan KS, Fahs CA, Ranadive SM, et al. . L-arginine as a nutritional prophylaxis against vascular endothelial dysfunction with aging. . J Cardiovasc Pharmacol Ther.. 2010 Mar;15(1):17-23. Epub 2010 Jan 6. PMID: 20053922 . ↑
Abstract - Zajac A, Poprzecki S, Zebrowska A, et al. . Arginine and ornithine supplementation increases growth hormone and insulin-like growth factor-1 serum levels after heavy-resistance exercise in strength-trained athletes. . J Strength Cond Res. . 2010 Apr;24(4):1082-90. PMID: 20300016. ↑
Abstract - Arwert LI, Deijen JB, Drent ML. . Effects of an oral mixture containing glycine, glutamine and niacin on memory, GH and IGF-I secretion in middle-aged and elderly subjects. . Nutr Neurosci. . 2003 Oct;6(5):269-75. PMID: 14609312. ↑
Abstract - Cynober L.. Ornithine alpha-ketoglutarate as a potent precursor of arginine and nitric oxide: a new job for an old friend.. J Nutr. . 2004 Oct;134(10 Suppl):2858S-2862S; discussion 2895S. PMID: 15465801. ↑
Abstract - Wideman L, Weltman JY, Hartman ML, et al. . Growth hormone release during acute and chronic aerobic and resistance exercise: recent findings. . Sports Med. . 2002;32(15):987-1004. PMID: 12457419. ↑
Abstract - Stokes KA, Sykes D, Gilbert KL, et al.. Brief, high intensity exercise alters serum ghrelin and growth hormone concentrations but not IGF-I, IGF-II or IGF-I bioactivity. . Growth Horm IGF Res. . 2010 Aug;20(4):289-94. Epub 2010 May 15. PMID: 20472480. ↑
Abstract - Pyka G, Wiswell RA, Marcus R.. Age-dependent effect of resistance exercise on growth hormone secretion in people. . J Clin Endocrinol Metab. . 1992 Aug;75(2):404-7. PMID: 1639942. ↑
Abstract - Møller N, Jørgensen JO. . Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. . Endocr Rev. . 2009 Apr;30(2):152-77. Epub 2009 Feb 24. PMID: 19240267 . ↑
Abstract - Meinhardt UJ, Ho KK.. Modulation of growth hormone action by sex steroids. . Clin Endocrinol (Oxf). . 2006 Oct;65(4):413-22. PMID: 16984231. ↑
Abstract - Root AW, Root MJ. . Clinical pharmacology of human growth hormone and its secretagogues. . Curr Drug Targets Immune Endocr Metabol Disord. . 2002 Apr;2(1):27-52. PMID: 12477295. ↑
Abstract - Takechi M, Tatehara S, Satomura K, et al. . Effect of FGF-2 and melatonin on implant bone healing: a histomorphometric study. . J Mater Sci Mater Med.. 2008 Aug;19(8):2949-52. Epub 2008 Mar 24. PMID: 18360797. ↑
Abstract - Van Cauter E, Copinschi G.. Interrelationships between growth hormone and sleep.. Growth Horm IGF Res.. 2000 Apr;10 Suppl B:S57-62. PMID: 10984255.. ↑
Abstract - Jones D., . Chapter 32: Clinical Approaches to Hormonal and Neuroendocrine Imbalances, . Textbook of Functional Medicine, ed. . Institute for Functional Medicine: Gig Harbor, WA, 2005, p. 644-668.. ↑
- Ristic-Medic D, Piskackova Z, Hooper L, et al. . Methods of assessment of iodine status in humans: a systematic review.. Am J Clin Nutr. . 2009 Jun;89(6):2052S-2069S. Epub 2009 May 6. PMID: 19420096. ↑
Abstract - Thomson CD, Chisholm A, McLachlan SK, et al. . Brazil nuts: an effective way to improve selenium status. . Am J Clin Nutr.. 2008 Feb;87(2):379-84. PMID: 18258628. ↑
Abstract - Gladyshev VN. . Selenoproteins and selenoproteomes. . In: Hatfield DL, Berry MJ, Gladyshev VN, eds. Selenium: Its molecular biology and role in human health. . 2nd ed. New York: Springer; 2006:99-114.. ↑
- Rayman MP.. The importance of selenium to human health. . Lancet. . 2000 Jul 15;356(9225):233-41. PMID: 10963212. ↑
Abstract - Burk RF. . Selenium, an antioxidant nutrient.. Nutr Clin Care. . 2002 Mar-Apr;5(2):75-9. PMID: 12134713. ↑
Abstract - [No authors listed] . High sodium-to-potassium ratio increases cardiac event risk. Study underscore the importance of balanced mineral intake.. Heart Advis.. 2009 Apr;12(4):5. PMID: 20383901. ↑
Abstract - Suter PM, Sierro C, Vetter W.. Nutritional factors in the control of blood pressure and hypertension. . Nutr Clin Care. . 2002 Jan-Feb;5(1):9-19. PMID: 12134718. ↑
Abstract - Hooper L, Bartlett C, Davey Smith G, et al. . Reduced dietary salt for prevention of cardiovascular disease. . Cochrane Database Syst Rev.. 2003;(3):CD003656. PMID: 12917977. ↑
Abstract - Hooper L, Bartlett C, Davey Smith G, e t al. . Systematic review of long term effects of advice to reduce dietary salt in adults. . BMJ. . 2002 Sep 21;325(7365):628. PMID: 12242173. ↑
Abstract - He FJ, MacGregor GA. . Effect of longer-term modest salt reduction on blood pressure. . Cochrane Database Syst Rev. . 2004;(3):CD004937. PMID: 15266549. ↑
Abstract - Om AS, Chung KW. . Dietary zinc deficiency alters 5 alpha-reduction and aromatization of testosterone and androgen and estrogen receptors in rat liver. . J Nutr. . 1996 Apr;126(4):842-8. PMID: 8613886. ↑
Abstract - Stamatiadis D, Bulteau-Portois MC, Mowszowicz I. . Inhibition of 5 alpha-reductase activity in human skin by zinc and azelaic acid. . Br J Dermatol. . 1988 Nov;119(5):627-32. PMID: 3207614. ↑
Abstract - Pham H, Ziboh VA. . 5 alpha-reductase-catalyzed conversion of testosterone to dihydrotestosterone is increased in prostatic adenocarcinoma cells: suppression by 15-lipoxygenase metabolites of gamma-linolenic and eicosape. J Steroid Biochem Mol Biol. . 2002 Nov;82(4-5):393-400. PMID: 12589947. ↑
Abstract - Lou YR, Murtola T, Tuohimaa P. . Regulation of aromatase and 5alpha-reductase by 25-hydroxyvitamin D(3), 1alpha,25-dihydroxyvitamin D(3), dexamethasone and progesterone in prostate cancer cells. . J Steroid Biochem Mol Biol.. 2005 Feb;94(1-3):151-7. Epub 2005 Feb 17. PMID: 15862960. ↑
Abstract - Habib FK, Ross M, Ho CK, et al. . Serenoa repens (Permixon) inhibits the 5alpha-reductase activity of human prostate cancer cell lines without interfering with PSA expression. . Int J Cancer, . 2005 Mar 20;114(2):190-4. PMID: 15543614. ↑
Abstract - Bratoeff E, Segura T, Recillas S, et al. . Aromatic esters of progesterone as 5alpha-reductase and prostate growth inhibitors. . J Enzyme Inhib Med Chem. . 2009 Jun;24(3):655-62. PMID: 18825535. ↑
Abstract - Bratoeff E, Zambrano A, Heuze I, et al. . Synthesis and biological activity of progesterone derivatives as 5alpha-reductase inhibitors, and their effect on hamster prostate weight. . J Enzyme Inhib Med Chem.. 2010 Jun;25(3):306-11. PMID: 19874206. ↑
Abstract - Park JS, Yeom MH, Park WS, et al. . Enzymatic hydrolysis of green tea seed extract and its activity on 5alpha-reductase inhibition. . Biosci Biotechnol Biochem. . 2006 Feb;70(2):387-94. PMID: 16495654. ↑
Abstract - Thompson IM, Goodman PJ, Tangen CM, et al. . The influence of finasteride on the development of prostate cancer. . N Engl J Med. . 2003 Jul 17;349(3):215-24. Epub 2003 Jun 24. PMID: 12824459. ↑
Abstract - Lyon M, Bland J, Jones D. . Chapter 31: Clinical Approaches to Detoxification and Biotransformation . Textbook of Functional Medicine, . Institute for Functional Medicine, Gig Harbor, WA, 2005, p. 564. PMID: 18825535. ↑
- Nishikawa T, Saito J, Omura M. . Prevalence of primary aldosteronism: should we screen for primary aldosteronism before treating hypertensive patients with medication? . Endocr J. . 2007 Aug;54(4):487-95. Epub 2006 Nov 24. PMID: 17124364. ↑
Abstract

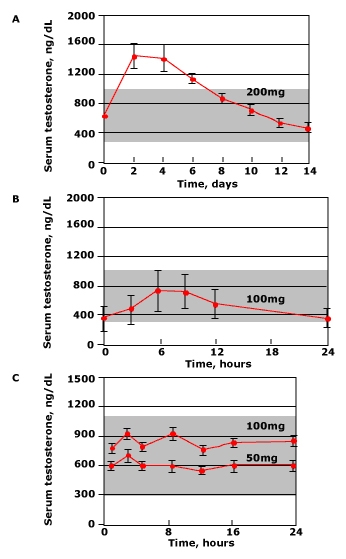
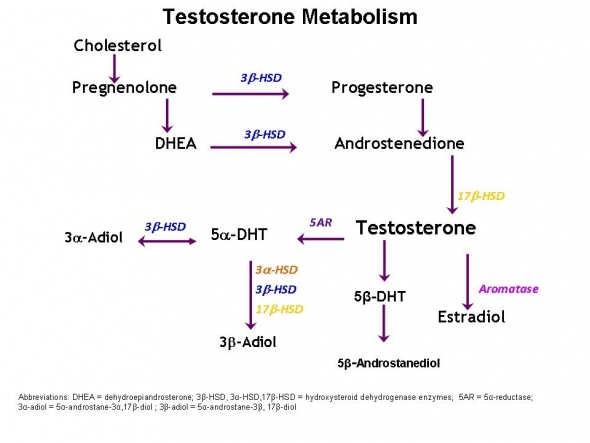
Comments are closed.